ABOUT BOWEL CANCER
Ostomy information
Living with a colostomy or ileostomy after a bowel cancer operation will require some adjustment. These changes are manageable and with education and guidance, you can return to a healthy, functioning lifestyle.
It’s normal to feel uncertain about how life will be after your ileostomy or colostomy
“Will I be able to do all the things I did before? Can I go back to work, swim, play sports, travel, and be as active as I used to be?”
It’s natural to have hesitations and concerns and we hope we will provide some answers, ideas, and helpful information. You’ll probably have lots of questions too and don’t be afraid to ask them because knowledge, experience, and support can help you gain confidence in this ‘new normal’ and live fully with resilience and strength.

Your surgery
Hundreds of people of all ages undergo ostomy surgery each year as a result of complications from a variety of diseases and conditions. Some diseases such as bowel cancer may require the surgical removal of affected portions of the bowel.
An ostomy is a surgically created opening on the surface of the abdomen (a stoma) allowing for the discharge of body waste (faeces) that can no longer pass through the bowel in the usual way. The waste output is collected in an external pouch (also known as a ‘bag’ or a ‘stoma appliance’, we use the word ‘pouch’).
We will focus on the ileostomy and the colostomy. These surgical procedures may be needed to:
- Allow post-surgical healing of the small intestine or colon (for example, if a section of the bowel has been removed as treatment for bowel cancer)
- Relieve symptoms of ulcerative colitis, Crohn’s disease and familial polyposis
- Enable complex surgery of the anus or rectum
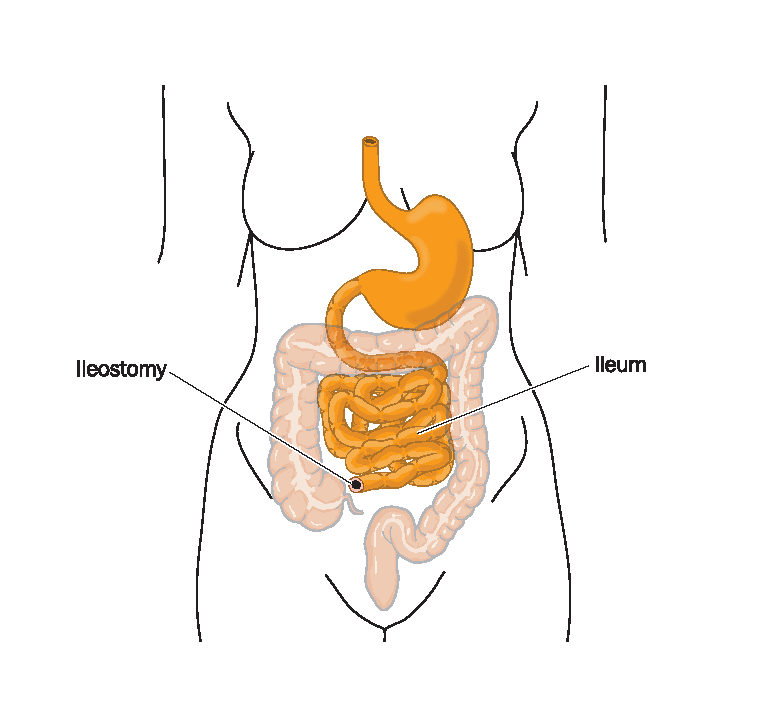
The ileostomy
A surgically created opening in the ileum (lowest part of the small intestine) is brought through an opening in the abdominal wall (made during surgery) to form a stoma, usually on the lower right side of the abdomen. An ileostomy may be temporary to allow for healing or rest of the small intestine or colon, or to enable more complex surgery of the anus or rectum. An ileostomy may also be permanent, depending on the individual circumstances.
After an ileostomy, digestive waste no longer leaves the body through the rectum and anus. It now exits through the stoma. This constant drainage is collected in a pouch that adheres to the skin around the stoma. The pouch is worn at all times and is emptied as needed. There are two main types of ileostomy, the loop ileostomy, and the end ileostomy. In some cases, it may be possible to have ileo-anal pouch surgery.
Loop ileostomy
During surgery, a loop of small intestine is brought out through a cut (incision) in your abdomen, opened up and stitched to the skin to form a stoma. The colon and rectum are left in place. The stoma will have two openings. They will be close together and you may not be able to see both. One of the openings is connected to the functioning part of your bowel (where waste products leave your body) and the other is connected to the inactive part of your bowel that leads to your rectum. The loop ileostomy is usually temporary and may be surgically reversed at a later date.
End ileostomy
During surgery, the ileum is separated from the colon and brought out through the abdomen to form a stoma. The stitches dissolve over time and the stoma heals onto the skin. Waste material comes out of the opening in the abdomen and is collected in a pouch fitted over the stoma. The end ileostomy is usually permanent.
Ileo-anal pouch
In some cases, it may be possible to have ileoanal pouch surgery (also called a J-pouch). This procedure involves the removal if the entire large bowel down to the anus and the creation of a new internal reservoir where the rectum used to be. The anal sphincter muscles are kept. A pouch in the shape of a J is made from the small bowel and attached to the anus. The pouch stores waste until you need to have a motion and the waste passes in the normal way. The area around the pouch requires healing so a temporary loop ileostomy is made above the pouch and a second operation a few months later will reverse the loop ileostomy.
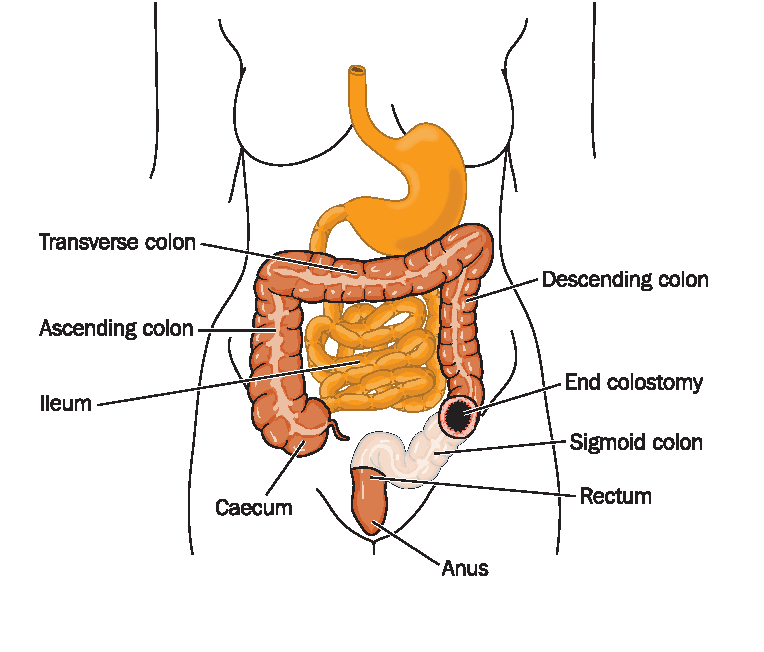
The colostomy
A surgically created opening in the colon is brought through the abdominal wall to form a stoma. A colostomy may only be needed for a short time (3 – 6 months) but may also be permanent, depending on individual circumstances.
The location of the colostomy stoma depends on which part of the colon is affected. Some are on the right, or the left or the middle. The way the stoma looks depends on the type of colostomy the surgeon makes and on individual body differences.
A colostomy changes the way your body passes stool (faeces). After a colostomy, the intestines will work as they did before but the colon and rectum beyond the colostomy are disconnected or removed and the anus is no longer the exit for stool. However, the anus will still pass mucus from time to time and this is normal.
The normal function of the colon is to absorb water, move stool towards the anus, and store stool in the rectum until it passes out of the body. A colostomy affects this function. The higher up in the colon the colostomy is made, the shorter the colon and so it has less time to absorb water, making the stool softer or more liquid. A colostomy further down in the colon, near the rectum, will put out stool that has been in the intestine longer and may be more solid or formed. After surgery, some people may still feel an urge to have a motion and may have some discharge from the anus such as mucus, blood, or stool left from the operation. If the rectum remains after surgery, it will continue to put out mucus that can be passed without harm when you have the urge. The type of colostomy used will depend on your circumstances.
Loop colostomy
This procedure is often used if the colostomy is temporary as it’s easier to reverse. During surgery, a loop of the colon is brought out through a cut (incision) in your abdomen, opened up and stitched to your skin to form a stoma.
As with the loop ileostomy, the stoma has two openings close together, one connected to the functioning part of your bowel (where waste will leave your body) and the other to the inactive part of your bowel leading to your rectum. In some cases a support device (known as a rod or bridge) may be used to hold the loop of colon in place while healing. This is usually removed after a few days.
End colostomy
During surgery, one end of the colon is brought out through a cut in your abdomen and stitched to the skin to create a stoma. This type of colostomy is often permanent but can be temporary when used in emergencies to treat bowel obstructions, colon injuries or bowel cancer.
The stoma
The stoma is a surgically created hole in your abdomen. A piece of the bowel is brought through a small incision in the abdominal wall onto the skin surface. It is then turned back on itself like the cuff of a sleeve and stitched. Stomas can vary in size and location, depending on the individual.
‘Stoma’ comes from the Greek word for ‘mouth’ or ‘oral cavity’. Waste (faeces) that would normally pass through the rectum and anus (back passage) now exits through the stoma into a collection pouch worn on the outside of the body over the stoma. The ileostomy brings the last part of the small bowel (ileum) through the abdominal wall and the colostomy brings through part of the large bowel. Both procedures allow bodily waste (faeces/stool) to pass through the stoma.
A stoma may be permanent or reversible, depending on the individual’s circumstances, and it is not uncommon for the surgeon to request the advice of the Stoma Nurse when determining a suitable site for the stoma before surgery. Location can affect the care of your ostomy and the type of clothes you like to wear and consideration is given to skin folds, scars and other irregularities to ensure the optimal stoma position.
After surgery
Even though you knew you would have a stoma, waking up after surgery and realising it’s there can be a difficult transition for anyone. Add to this the normal stresses of surgery and you may feel many unexpected emotions, perhaps fear, sadness, and anger, just to name a few.
This is normal so allow yourself time to feel whatever you need to.
Chances are you were not too healthy prior to surgery, or a colonoscopy had revealed a problem. Waking up with a stoma and wearing a stoma pouch can be hard to take in but it is a positive step towards health and recovery.
Looking at your stoma for the first time may cause some emotion. Having your Stoma Nurse or someone you trust with you may help.
Your Stoma Nurse
While in hospital, your Stoma Nurse will show you how to care for your ileostomy or colostomy. The Nurse is a qualified professional with additional training in all aspects of this type of post-operative care and will be able to assist you before, during and after your ostomy.
Most large hospitals will have a Stoma Nurse and smaller facilities may employ a nurse in a part-time dual position.
Your Stoma Nurse remains your primary contact for information, support, for ordering your stoma supplies and assisting with the ongoing management of your stoma.
Caring for the stoma
The stoma may look large at first but will shrink to its final size about 6 to 8 weeks post-surgery. The shape will be round to oval. It may stick out a little or be flat against the skin. The stoma will look pink to red in colour and appear moist. A stoma bleeds easily if it is rubbed too hard and can be particularly sensitive in the early months post-surgery. Any bleeding should stop quickly but if it persists or if blood is coming from within the stoma, contact your Stoma Nurse right away.
There are no nerve endings in the stoma so it will not be painful or feel uncomfortable. There may also be a ‘bridge’ (supporting rod) going underneath the stoma to support it for the first few days.
When you wake up after surgery, you will be wearing your first pouch. It will most likely be a clear pouch so the Stoma Nurse attending you can check your new stoma easily.
Your stoma will begin to work within a few days post-surgery. The initial output may be watery and strong smelling as your bowel hasn’t been working for a while. There may be a small amount of blood and some wind (flatus) may come from the stoma too. These are all normal effects and will settle. Make sure to drink plenty of water during this time to avoid dehydration. Your doctor will let you know when you can eat and drink as usual.
Patients who still have some lower bowel (rectum) may feel the need to go to the toilet as before and pass some blood and mucus. This is normal and it may help to sit on the toilet to help the mucus pass.
Keeping a stoma diary can help you track your recovery, stoma appearance, and output from the stoma. You can note any changes in size and colour, any issues with the surrounding skin (redness or irritation), and you can write down any questions you may have for your Stoma Nurse or doctor.
The ileostomy/colostomy pouch
After your operation, faeces will pass through the stoma. Unlike the anus, the stoma has no shut-off sphincter muscle or valve so you will not be able to control the faeces passing from the stoma.
An ileostomy/colostomy pouch collects the faeces as it passes through the stoma. There are several different types of pouches and your Stoma Nurse will show you the ones that are best for you.
Faeces is often quite watery in the first few days after surgery. Your Stoma Nurse will help with emptying the bag and other tasks until you are ready and have learned how to do it for yourself.
The pouch sticks onto your abdomen, over the stoma, and has a filter that releases wind (flatus) so the pouch will not inflate (called ‘ballooning’) and a deodorizing action to minimise odour. The pouch is waterproof and can be worn while showering or bathing.
For further information please download our resource.


