ABOUT BOWEL CANCER
Polyps
Many people have small growths in the bowel, called polyps. They’re mostly harmless and rarely cause symptoms so you may not know you have them.
However, some polyps can develop into bowel cancer over time, so it’s a good idea to have them monitored and removed if they show signs of becoming malignant.
What are polyps?
Bowel polyps are small growths on the inner lining of the large intestine (colon) or rectum.
- They are very common, affecting around one in four people aged 50 or over, as well as many younger people.
- They’re slightly more common in men.
- Some people develop just one polyp while others have many.
- Most polyps are harmless; however, some can develop into a cancer.
Bowel polyps do not generally cause symptoms, so most people won’t know they have them. However, they are often picked up during regular screening for bowel cancer which checks for tiny traces of blood in your poo. This is why it is important to participate in the free government-run National Bowel Screening Programme when you are sent a test between the ages of 60 and 74, or to continue with any other screening suggested by your specialist or healthcare provider.
Larger polyps can cause the following symptoms:
- Small amounts of mucous or blood in your poo.
- Diarrhoea or constipation.
- Abdominal pain.
Polyps are usually benign (i.e., non-cancerous). However, it’s important to remove polyps because if they are left, they may become malignant (i.e., cancerous).
There is a specific type of polyp that is more likely to become cancerous, known as an adenoma polyp. It is thought that one in 10 adenoma polyps may change over a period of 5 to 10 years and become a cancer.
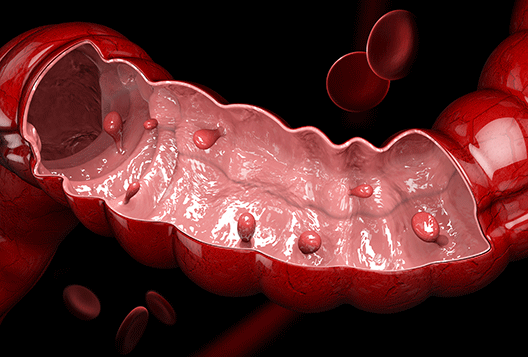
What does a polyp look like?
The polyp growth can be on a stalk and look a little like a mushroom – these are called pedunculated polyps. Alternatively, they can be quite flat to the surface of the bowel with a broad base known as sessile polyps.
Polyps can be anything from a few millimetres to a few centimetres in size. The smaller the polyp, the less likely it is to become cancerous.
What are the risk factors?
The risk factors associated with polyps are similar to those for bowel cancer. Risks increase for those over the age of 60, smokers, those who have a sedentary lifestyle, and where there is a genetic predisposition to polyps.
What causes bowel polyps?
The lining of the bowel is constantly renewing itself. Worn-out cells die and are shed, with new cells taking their place. Each cell has the genetic information needed to do its specific job. If this information becomes faulty, it may cause cells to grow more quickly and with slightly different qualities.
The exact cause is unknown. However, it is thought that polyps may develop due to the body producing too many cells in the lining of the bowel. It is these extra cells that then form a polyp.
You may be more likely to develop these polyps if:
- A member of your family has had bowel polyps or bowel cancer.
- You or a member of your family has a hereditary condition which may cause many polyps to develop.
- You have a condition that affects your gut, such as Inflammatory Bowel Syndrome (IBS), Colitis or Crohn’s disease.
- You are overweight.
- You are a smoker.
How are polyps diagnosed?
Polyps are commonly diagnosed during a colonoscopy. Although stool sample kits may reveal small traces of blood, which could be from polyps, the only sure way to find them is from a colonoscopy/sigmoidoscopy or CT colonography.
CT colonography can identify polyps larger than 5mm within the bowel. The next step is to be referred for a colonoscopy.
During a colonoscopy, surgeons can take a good look at the entire length of the bowel. They can check for polyps and remove any they find.
How are polyps removed?
During a colonoscopy, most polyps are removed by passing a wire through the endoscope and looping the wire around the polyp – like a lasso – to remove it. This is quite painless, and only one procedure is usually needed to clear the bowel of polyps. It usually takes place during a day visit to a clinic or hospital.
Occasionally there are too many polyps to be removed safely during a single visit, so the procedure would need to be repeated.
You may be advised to have regular colonoscopy procedures every 2 to 5 years, depending on how many polyps were detected and removed.
What happens after the polyps are removed?
They are sent to the laboratory for analysis. This will show whether a polyp has been completely removed and also whether it had the potential to become a cancer. In addition, the lab can check that cancer has not already developed.
If the lab finds there was a cancer developing in the polyp, you may need further treatment, depending on the type of cancerous change found. Your specialist will talk with you about this.
Remember, in the vast majority of cases the polyps are harmless. They are simply removed, and you can carry on with normal life. You may be advised to have regular colonoscopy checks every 2 to 5 years to see if there are any more polyps that need to be removed.
Hereditary causes of polyps
- Lynch syndrome. Also called hereditary nonpolyposis colorectal cancer. People with Lynch syndrome tend to develop relatively few colon polyps, but those polyps can quickly become malignant. Lynch syndrome is the most common form of inherited bowel cancer and is also associated with tumours in the breast, stomach, small intestine, urinary tract and ovaries.
- Familial Adenomatous Polyposis (FAP) This is a rare disorder that causes hundreds or even thousands of polyps to develop in the lining of the colon. It can begin during your teenage years. If the polyps aren’t treated, your risk of bowel cancer is nearly 100%, usually before the age of 40. Genetic testing can help determine your risk of FAP.
- Serrated polyposis syndrome. This is a condition that leads to multiple serrated adenomatous polyps in the upper part (right side) of the bowel. These polyps have the potential to become cancerous and require monitoring and removal.
There are some other conditions that are similar to FAP but are much rarer.
Summary
Polyps are small growths in the lining of the bowel that are very common. They usually don’t cause symptoms and are usually harmless in themselves. However, a polyp may start to change in a way that causes bowel cancer, so it’s important to take part in regular screening programmes as you grow older and if you have any of the risk factors covered above.
