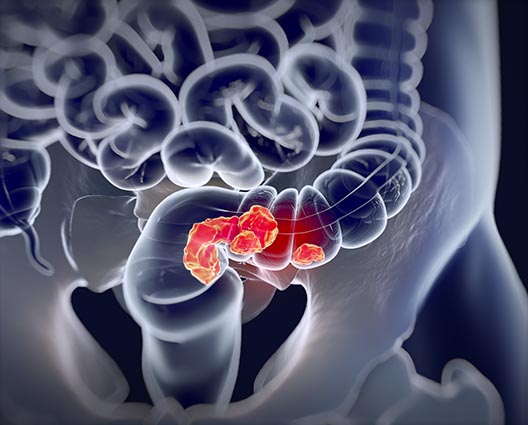
ABOUT BOWEL CANCER
Rectal Cancer
The rectum is the last 12 centimetres of the large intestine. Rectal cancer begins in the innermost lining of the bowel called the mucosa. Adenocarcinoma of the rectum generally grows slowly. A long time may pass before it becomes large enough to cause symptoms.
Cancer of the rectum should be considered whenever there is rectal bleeding, even if other causes, such as haemorrhoids, are present.
Thirty per cent of all colorectal tumours develop in the rectum; however, in patients under 50 years of age, it may account for half of all bowel cancers and is increasing rapidly.
What are the risk factors of rectal cancer?
Risk factors tend to be similar to those for colon cancer which include:
- Sedentary lifestyle
- Diet high in red and/or processed meat
- Smoking
- Higher than recommended alcohol intake
- High sugar and processed foods diet
Other things to take into account for rectal cancer can include non-cancerous bowel health issues such as:
- Inflammatory bowel disease for example: Ulcerative Colitis, Crohn’s disease, Diverticulitis
- Type 2 diabetes
- Benign colorectal polyps
- Lynch Syndrome
- Familiar adenomatous polyposis (FAP)
Of course, each person’s risk profile is unique. The insight oncologists currently have into colorectal cancer risk factors is based on studies of past patients, and there is no way to predict whether a specific person will develop rectal cancer in the future. Also, if cancer does develop, there is no way to determine if it is the direct result of a specific risk factor or trigger. With this in mind, risk factor information is best used to identify specific individuals who should participate in more frequent colorectal cancer screenings than the general population.
What are the symptoms of rectal cancer?
Symptoms for both colon and rectal cancer are similar including:
- Changes to bowel habits which continue over several weeks
- Stomach or gas pains
- Constipation or diarrhoea (or both)
- Black, dark, or red-coloured stools, can all indicate blood
- Feeling weak, tired or short of breath
- Feeling an incomplete emptying of bowels
Symptoms of advanced disease can include:
- A feeling of being full very quickly while eating
- Weakness and pain in the abdominal area
When symptoms do occur, they vary depending on the location of the tumour, its type, how far it has spread and complications it may have caused. Routine exams such as abdominal palpation, rectal exam and blood tests (to check for anaemia) are important for early diagnosis.
What are stages of rectal cancer?
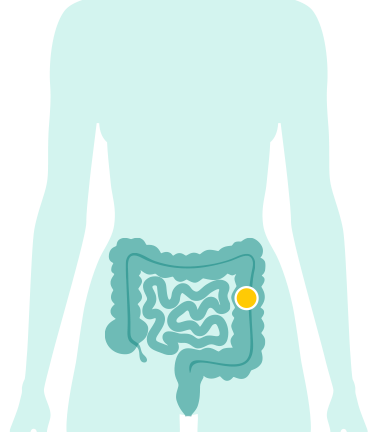
Stage I (1)
The cancer hasn’t spread outside the bowel wall.
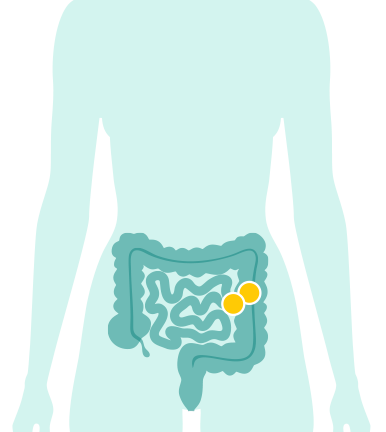
Stage II (2)
The cancer has grown into or through the outer layer of the bowel wall.
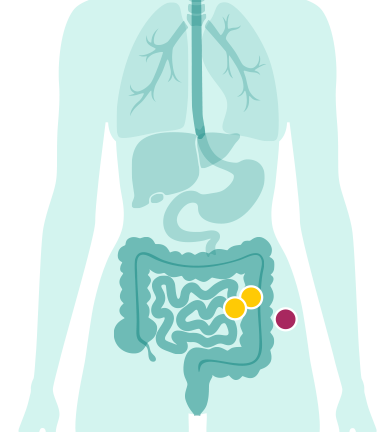
Stage III (3)
The cancer has spread to nearby lymph nodes.
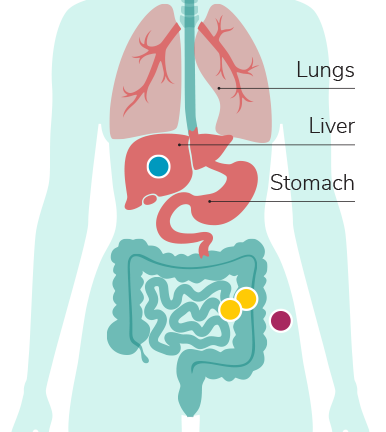
Stage IV (4)
The cancer has spread to other parts of the body – often the liver or lungs. This is known as metastatic bowel cancer.

What are the treatments for rectal cancer?
Treatment of rectal cancer depends on how far the tumour has spread and how close it is to the rectum. A combination of radiation therapy and chemotherapy may be helpful for rectal cancer patients. Most patients with early rectal cancer can be adequately managed by surgery alone.
You are likely to have surgery for rectal cancer, during which your surgeon will try to cut out any tissue affected by cancer without removing the anal sphincter muscle, which controls the opening and closing of the anus during bowel movements. But in some cases, a rectal tumour is too close to the muscle to save it. In that case, you’ll need a colostomy.
About 1 in 8 people with rectal cancer will need a colostomy formed during surgery, which may well be temporary.
Neoadjuvant therapy for rectal cancer often involves the use of pre-operative radiotherapy to help shrink tumour size when looking for curative treatment. This may be used in conjunction with chemotherapy or alone. This type of treatment plan is often used with locally advanced disease (where it has spread to neighbouring lymph node, but not metastasized to other organs) This type of therapy is useful for down staging of tumours and helping to make surgery less invasive and minimizing risk of having to remove larger portions of the bowel/rectum.

Some patients completely respond to radiotherapy and have been enrolled in surveillance programmes without undergoing surgery. It is essential to be aware of the disadvantages associated with radiotherapy. Radiation therapy increases the risk of anorectal and genitourinary dysfunction which can have a marked effect on the quality of life for some.
