SUPPORT
Jan’s Journey: Surviving Bowel Cancer and Giving Back One Snood at a Time
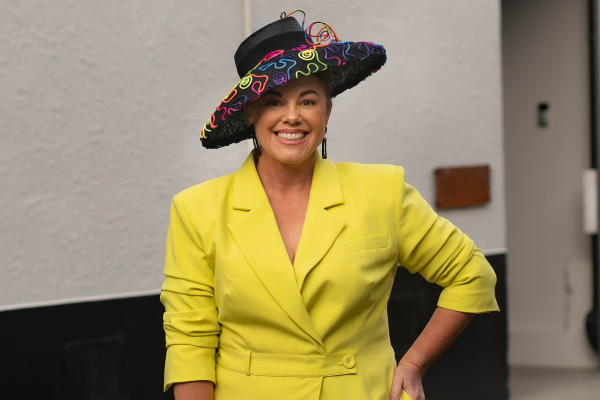
 Jan (left) with her sister Lynn
Jan (left) with her sister Lynn
“If it wasn’t for BCNZ I wouldn’t be here – simple as that.”
“In October 2019 (just before covid), my young sister, Lynne was in Auckland for work. Going to an appointment she was following a bus with an advertisement on the back for BCNZ saying ‘Never Too Young to get Bowel Cancer’. As she followed it for quite a while, her eyes kept going back to the advertisement. She thought ‘this is a sign!’.
It continued to play on Lynne’s mind. Being in her 50’s and having a history of bowel cancer in our family, Lynne decided to have a colonoscopy when she returned home. They found nine cancerous polyps and the surgeon suggested she tell her family to get checked too – I thought about it for a while, but because I had no symptoms I decided I would talk it over with my GP at my next doctor’s appointment.
After chatting with my doctor, they decided to refer me for a colonoscopy, but it would cost me almost $3000.
I had my colonoscopy in November 2019, and to everyone’s shock (because I had no symptoms), I was diagnosed with bowel cancer. I was operated on in early December 2019. The surgeon said if I hadn’t had the operation I wouldn’t have made it to the following Christmas”.
Grateful for the second chance, Jan, along with her family and friends, turned her hands to knitting snoods for bowel cancer patients to wear while going through chemotherapy and when they experienced hair loss – each available for a $20 donation to support the cause.”

“Now we knit snoods and dish/face cloths, and I sell them at the local markets to raise money for BCNZ. I started knitting these because there isn’t a big need for snoods in the summer.”

Jan with her amazing team of friends and family
To date, me and my team of knitters have raised nearly $5,000 from the snoods and cloths!
In addition, my husband Doug has raised around $6,000 through Move your Butt and doing various fundraising walks.
Huge thanks to Jan and her friends and family for turning a tough experience into something so generous!
You can support Jan’s beautiful work by donating to her fundraiser and choosing your own hand-knitted snood or cloth. Simply make a donation through her fundraising page below.
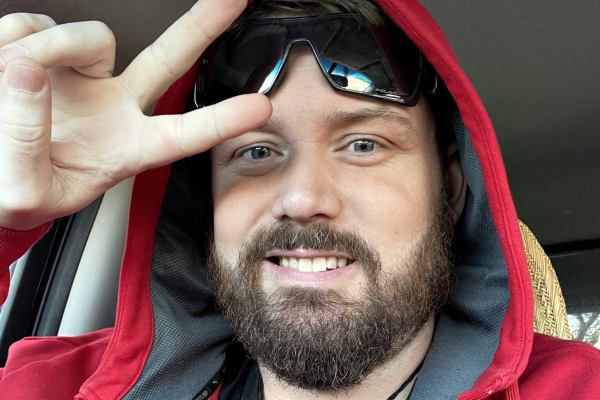
“Brighter Days Are Coming”: Oscar’s Journey with Bowel Cancer

“I had abdominal cramps, mostly on the right side of my bowel. I went to see my GP in June 2021 in the UK complaining about the pain I was experiencing, and they did some blood tests, but nothing sinister showed on the results. I carried on since the blood was ‘normal’, but boy, how wrong was I?
In December 2021, the pain was excruciating, and I started vomiting now and again. Little did I know this was food being blocked. The doctor put it down to IBS. I was prescribed some Mebeverin and peppermint tablets to help with the cramps and the IBS. Finally, in March 2022, my GP requested I get a FIT done, and that’s when everything turned upside down. The test came back positive for bowel cancer.
I had a colonoscopy done on April 10, 2022, and they saw a tumour, about 5 cm in size. I had a CT scan and an MRI scan in late April 2022, and both confirmed I had bowel cancer. It wasn’t a shock, as the FIT had kind of prepared me for the news. Luckily, at the time, it was local. I had a right hemicolectomy to remove the tumour on May 24, 2022. The histology result showed one of my lymph nodes had cancerous cells. I was advised that I would need chemotherapy.
I started my 12 cycles of FOLFOX on July 12, 2022. That ended in February 2023. The delay was due to neuropathy and neutropenia. I had a scan on my birthday in March, and two weeks later, the results came back as no evidence of disease (NED). I thought I had seen the back of it. I had a colonoscopy in July 2023, and it came back okay. Fast forward to August 2023, and my CEA test showed a rise in the markers. I had a CT scan again, and that came back NED. The surgeon sent me to Oxford for a specialist PET/CT scan in September 2023, and it showed glucose uptake on the anastomosis joint in the bowel. I then had a colonoscopy again, and the samples were benign. It was a relief. I had another CT scan in February 2024 and again, NED. The doctor advised I have an MRI scan just to make sure things were okay inside.
I came to New Zealand because my partner was already here. I then had the MRI done in April 2024. I had my results on May 6, 2024. The doctor said you have cancerous activity on your liver and around the abdomen.
It was a shock, as all my scans had been showing NED. It was not the news I wanted to hear, but I had to accept it and get on with it. In May 2024, I had a PET/CT scan again, and it pretty much confirmed what the MRI had shown. I was referred to clinical oncology. I started my second-line treatment of FOLFIRI on July 12, 2024. The oncologist also advised that I get Avastin, and unfortunately, that isn’t funded here. I am in the process of raising some of the funds via GiveaLittle. In September 2024, the CT scan showed progression, a very concerning scenario. In October 2024, I started Avastin as an extra to FOLFIRI.
I had a CT scan in November 2024 and had the result in December, and that showed that Avastin was working well since tumours reduced in size and there was no new metastatic disease. I am currently having the treatment, and my CEA is dropping at a slow pace because I have low volume disease. Long may it continue. My latest CT scan done in March 2025 shows no progression, tumours are shrinking, and CEA markers are coming down. I am responding well to treatment, which is a relief.
My oncologist said I would be in a really bad situation had I not started Avastin. Longevity has its place in life, and like anybody, I would like to live. I worry about the unsustainability of paying for the drug in the long-term.
It is hard. This disease doesn’t discriminate whether you are young or old. It seems a lot of us younger people are on the receiving end of it.
In my free time, I find passion in computer coding, mathematics with Python and Maple and reading on my Kindle.
To all those going through this disease, we got this. Brighter days are coming. Hopefully, there will be better-funded drugs in the future. To our carers and crowdfunding donors, thank you for your support. Misfortune doesn’t mean it is all over, after all, adversity builds resilience. There’s always hope. Remember, every storm eventually runs out of rain. Keep smiling”.

Nurse for 40 years, always encouraged my patients to do the Bowel Screening Test
“My bowel screening kit arrived on my 60th birthday and I returned it completed in a couple of days and then forgot about it. I had no symptoms, and a recent blood test indicated I was not anaemic.
A week later whilst working as a Practice Nurse the phone rang, and it was my GP. He said my bowel screening test came back positive and he had booked me in for a colonoscopy.
I was seen about 4 weeks later and on the day of the procedure I was told that I had descending sigmoid colon cancer. My doctor husband and I were in tears. I then went through a series of tests that indicated I had a secondary in my liver. How could this be so? I was carrying these nasty passengers without any awareness of illness.
I have now met my two surgeons who are going to operate on me in one session. Both tumours will be staged after the event, and I will be informed if I need chemotherapy and, or radiotherapy.
My message is I am so glad the age for bowel screening is coming down and thank you to Time to Screen for providing these bowel screening kits.”
Dawn’s Story

“At age 44 I was diagnosed with stage 3b bowel cancer.
Without chemo my oncologist gave me 10% chance of survival. With chemo, a 30% chance.
I had no prior symptoms and no family history but following three days of debilitating pain and four hospital visits, a CT scan found my fist size tumour and I had 15 minutes notice of my emergency surgery to remove three feet of my colon and 32 lymph nodes. I woke with a colostomy bag and after a week in Rotorua hospital, I was air ambulanced back to Christchurch hospital for another week before I was released. Chemo started three weeks later.
In my journey through the challenges of bowel cancer, I’ve discovered a newfound appreciation for life’s precious moments. Three years ago, the diagnosis could have defined me, but instead, it ignited a fire within me to live life to its fullest. My wonderful surgeon, Dr Frank Frizzell and his team have backed me as a survivor from the start! He told me to go live the hell out of life. So I am.
As a chef, I’ve always found joy in creating culinary delights that bring people together. Despite the hurdles of my health journey, I continue to infuse passion and flavour, sharing my love for food and spreading positivity one meal at a time. My role as Head of Food Development for 20 cafes in the Coffee Culture franchise keeps me busy but basically, I’m paid to eat cake!
Beyond the kitchen, my heart finds solace and purpose in caring for animals at my 32-acre foster farm. Each day, I’m reminded of the healing power of compassion as I provide a loving sanctuary for rescued animals, advocating for their welfare and happiness.
During the six months of chemo where I became malnourished, I had good days and some not so good. On the good days I might have an hour or two of energy to sow some seeds in a small indoor plastic grow house. Even just going through my seed collection brought me joy and spurred me on to get through these trials and back on my plot. Back to the animals on my 32 acres and to my majestic tunnelhouse.
I couldn’t wait to once again grow most of what I ate and nourish my body, mind and soul.
I did seed swaps with strangers through the post. I would fold origami seed envelopes to pass the time. I read and educated myself on the parts of gardening that I wasn’t yet proficient at.
Being limited to not lifting over 5kg made being on my land impossible so I destocked the majority of my animals and had friends tend to the ones I kept. My support circle were incredible. Missing lambing and kidding season was tough, but I knew I’d be able to be back there, in my happy place, soon.
The chemo infusion I had every three weeks, followed by two weeks of taking 8 pills every 12 hours was gruelling. It gave me extreme cold sensitivity where breathing in cold air felt like shards of glass in my throat. Touching anything cold, even cutlery, would burn my skin. The soles of my feet burnt, blistered and peeled and my toe nails fell off. I didn’t go outside for the first ten days after a new cycle of chemo.
So even sowing seeds was tricky. But I did.
I believed in a glorious tomorrow where I would reap the benefits of those stolen minutes of productivity.After chemotherapy was concluded I had a months rest before my bowel reconstruction surgery so I made the most of a week where I felt really good. I transplanted seedlings like my life depended on it. And it may well have.
My tunnelhouse has automatic watering so once my precious babies were in my raised beds, technology and Mother Nature took over while I rested and recuperated after another tough hospital stay. This time I was only allowed to lift 1.5kg for 8 weeks until my wounds with 77 staples healed.
But just as spring sprung, my energy improved, my body healed and my dark cloud lifted as I returned to my land full time and got stuck in. My tomato plants needed their laterals removed. Fence lines needed weed whacking. And more seeds to sow.
Prior to being sick I use to work 65 hour weeks in the city, a 45 minute drive away each direction. My time spent on my land was minimal and rushed.
My surgeon told me to get on and live the hell out of life. My priorities changed. I became part of my community. Actually part of many different communities. I sought out young people who needed support with colostomy bags and cancer diagnosis. I mentored gardeners and kids. I studied gut health like it was my new religion. I reaped the rewards of my soil toil. And fed my community. And I believed in tomorrow! I’m not just surviving. I’m thriving!
I feel pretty honoured to be featured in three different gardening publications – Nz gardener magazine, 2023 Gardening Dairy and the Grow More, Spend Less magazine.
I stay active and eat well. Especially concentrating on great gut health.
I bike and hike but my latest obsession is pickleball. (Like little tennis)
Recently, I had the honour of winning a bronze medal in the women’s doubles A grade pickleball tournament in Canterbury. A testament that you can be resilience and have determination to thrive despite adversity. Following on from that win, I’m playing in another tournament in Auckland at the moment . I never thought this would be possible just a couple of years ago as I battled through treatment and numerous surgeries and procedures.
Through my journey, I’ve come to realize that every challenge is an opportunity for growth and every setback is a chance to rise stronger. I am Dawn Ballagh, not just a survivor, but a living testament to the power of resilience, the beauty of life beyond adversity, and the limitless possibilities that await when we choose to embrace each moment with gratitude and courage.
You can do this.
Feel free to follow my journey on instagram @travellin_gourmet. ”
Jenny’s Story

“I was diagnosed in November 2021 with stage 3 sigmoid colon cancer. My children were 6, 4 and 3 at the time and I thought I had haemorrhoids from childbirth. My GP was amazing and we monitoring for a month and did blood tests which came back as iron deficient so I went in for a colonoscopy and got the lift changing news.
I was in booked in to get surgery a week later and got the news it has spread to some lymph nodes that were removed but meant I needed to have chemotherapy afterwards. The next 6 months were a blur to be honest. I recovered from surgery and had a much quieter Christmas and then started Chemo on January the 10th. This was still in Covid times so it was very hard keeping away from friends and family to keep myself well which made me feel even more isolated.
My husband and Mum were amazing and took over the with kids so I could focus on myself to get through this but Mum guilt still rears its head that I had to miss the first day of school for my son and other key moments.
I managed to get through all 8 rounds of chemo but it got tougher and tougher and I still 2 years on have some of the side effects of neuropathy which I think will stay with me now.
Mentally it took a toll on my husband and I coming out the other side when you get told to “go back to normal” – your normal has changed forever along with priorities and how you view your life so that took time to deal with.
Overall now I am luckily that I don’t think about cancer on a daily basis now but reading o many stories of other young people getting diagnosed makes me hope we can get some research into why this maybe happening and also how we can support young families in these situations.
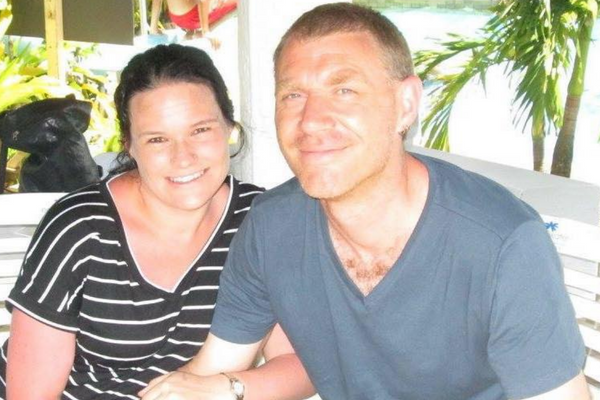
I don’t have too many photos during Chemo – but this one was taken in Rarotonga not long after I finished chemo. We booked it after my 6th round with 2 more sessions to go as we needed something fun to look forwards to at the end. We had such a great family time just relaxing and not thinking about anything medical for the first time in awhile! ”
Julia’s Story

“A massive stage III tumour was discovered with surgery 4 weeks later. If it wasn’t for my doctor taking that extra step toward the colonoscopy? I would likely be facing chemo, or death. It was 6 weeks from diagnosis to clearance. I consider myself one of the lucky ones.My BM’s started coming at odd times (middle of the night, during meals) and then after a few months of that, more frequent – with only a little bit at a time – never feeling completely “empty.” A few months later, small amounts – but loose. No pain, no blood. I booked a doc appt and all tests came back negative, but with “a little inflammation in the stool sample.” My doctor said it might be worth doing a colonoscopy – just to rule everything out.
It was a complete and utter shock to learn they’d found a massive tumour – especially given the tests hadn’t shown markers that necessarily point to cancer. The absence of pain and blood made me feel like it was more IBS or diverticulitis- or food allergy stuff. It was also over Xmas – so having to wait for MRIs and appts was so difficult- but I did have a great team at Taranaki Base who sprang into action as soon as they could. My surgery was successful, and a few weeks later they were able to confirm that the lymph nodes had been unaffected. No chemo necessary.
I just had my 2nd year CT scan and no cancer anywhere. My BM’s still come at odd times, and there’s certainly some trauma emotionally that I work through in psychotherapy, but otherwise – being in the clear feels incredibly lucky.
I learned a valuable lesson from my cancer. I had to stop everything and be taken care of by my partner, kids, extended family – and my community. I didn’t realize how much I was loved. What an incredible discovery!
I feel like I got lucky with a doctor who was as curious as I was – despite there being no direct cancer indicators, and encouraged a colonoscopy. Others won’t be as lucky, and may be rushed through an initial appt. Colonoscopies are the only true way of knowing what’s going on. “
Myra’s Story

“Because the toilet bowls fill up quite high in the US, when I turned to flush I noticed something in my poop that looked like dark red lines. When I got home I was in two minds about going to the doctors coz my symptoms were gone – but I did and because my grandfather had died of bowel cancer (which I didn’t realise until right then) I was put on a semi-urgent priority for a colonoscopy “”just to be safe””. 6 weeks later on 18 April 23, I saw my tumor on the big screen. I was stage 3 (in local lymph nodes).
My hubby was quiet but later said it was like someone punched a hole in his guts. We told our kids right away (ages 7 to 24).
On the June 6th I started 1 week of radiation at Palmy (we stayed at Ozanam House which is amazing). I was active, but after the 2nd radiotherapy session I was so sore in my hips and pain radiating down my legs. I had to go on serious painkillers. The murals in the radiotherapy rooms were soothing. I said karakia during every session but by the end I hated it.
I started chemo but my body rejected the oral pills and I had horrible diarrhea, was hospitalised and lost 5kg. I switched to folfox – got a port (highly recommend if you’ve got rubbish veins) and went until the end of November making friends with a bum bag #iykyk
Neurospathy was the worst in my mouth esp teeth. Post chemo it got worse in my fingers and toes and I’m still waiting for those symptoms to fade. I ate my way through chemo and was very fortunate that I work only part time from home so spent most of June to November at home with my family (and my food!).
My sigmoidiscopy and CT/MRI came back clear. It’s a miracle not lost on me as I lost a dear friend to cancer this year. I’m so thankful to the lovely nurses at Villa 6 (Hastings). The way I made it through was by being grateful for the little things, accepting help and not putting too much pressure on what I could achieve.”
Samantha’s Story

“The diagnosis: (Rectal carcinoma with group G streptococcal sepsis in the early third trimester)
I was diagnosed at the age of 26, with stage 3B bowel cancer, while I was 28 weeks pregnant with my son Lockie. The tumour filled my entire large bowel and perforated, going into the blood which resulted in Septicemia. They almost lost us both.
My son was delivered at 28 weeks 5 days old and spent 3.5 months in Neonatal Intensive Care Unit (NICU). Following the delivery, I was given an ileostomy (bag) to give my bowel a chance to rest while I had treatment. I had this for 377 days. This was quite hard to deal with later on but I didn’t really have time to think about it as it was straight into radiation and oral chemotherapy. There was a small window of opportunity and we just had to take it.
There was no time to pin ovaries or to freeze eggs for future children (I had severe endometriosis prior). I could never have any more children – Lockie was my miracle.
At the diagnosis stage, the tumour was too large, so an operation was off the table hence a 5-week stint of daily radiation and oral chemotherapy.
A few weeks later I had a setback as the little buggers got into my liver so I had a few rounds of Folfox before liver surgery. The hardest part of going into this surgery, was saying goodbye to my son, who I wasn’t sure if I’d ever see him again. My body was weak but I knew I had to fight for him.
I spent a lot of time in hospital, while my son was in NICU. I would rest all day to go down to NICU to spend time with and read to him. He was my fight and nothing has changed, 7.5 years later.
After the successful removal of the two cells in my liver, more chemotherapy followed in an effort to continue to shrink the tumour in my bowel. The tumour had shrunk by 75%. Due to my response to treatment, it had now made an impossible operation, possible.
The morning of the tumour removal was emotional, just like the liver surgery. I’ll never forget picking up my six-month-old son and saying goodbye. It was different this time. I held him in my arms, hugged him and kissed him. My heart broke but again I knew I had to maintain my determination and strength to keep fighting so I could see him again.
The tumour in my bowel was successfully removed and there was enough to rejoin. To finally have that out of my body, I still can’t describe that feeling.
An intensive monitoring period – CT scans, MRI scans, regular tumour marker blood tests (I felt like a pin cushion), countless specialist visits – followed. Once I’d finished my chemotherapy (the magic 12 rounds) the ileostomy reversal happened; and eventually appointments started to become further and further apart.
Receiving the ‘you are cancer free’ news definitely took a few minutes to sink in. A lot of happy tears and what felt like the largest weight I’d been carrying for five years, lifted. I am so grateful and so thankful to all the medical teams that were part of my journey. I felt as though I had the best of the best – from oncology to surgeons and support staff, fighting in my corner.
My diagnosis (Rectal carcinoma with group G streptococcal sepsis in the early third trimester) was published in the 2018 International Federation of Gynaecology and Obstetrics Journal.
I wanted to help and make sure that if anyone ever presented in similar circumstances to myself, they may have some idea of what a potential diagnosis might be.
As part of being a support person for those that are currently going through bowel cancer, I’ve been lucky enough to have formed wonderful friendships with the most incredible people that are giving everything they can and more to fight this cruel disease.
Being a support person isn’t easy, but this was one way I felt that I could give back. Sadly, I’ve lost my friends now, but they are also at peace which is a comfort. I’ll cherish the memories we made together, forever.
I’m now at seven years remission. I am thankful for every day.”” email to us – “”Trail Running is my happy place so I’ve attached a recent photo from a 34km trail run I completed in October.
The journey has been long and tough but anything I can do to help others going through this, including sharing my story, I will do it 😊
Thank you for putting the opportunity out there to share. It’s so important.”
Thomas’s Story

“In the summer of 2012 I wasn’t feeling well. I was tired. I went to my GP; she thought I had asthma and prescribed an inhaler. No improvement. I went back. She thought I was depressed and prescribed citalopram. No improvement, although I did yawn so much I thought I would dislocate my jaw. I went back yet again. This time she took some blood.
On a Saturday she rang and told me that I needed to get to Christchurch A&E as soon as possible. She said I was so anaemic she was surprised I was conscious and able to function.
So began Bowel Cancer Act I.
At Christchurch Hospital I was diagnosed with bowel cancer in my ascending colon. I met my surgeon; he performed a right hemi-colectomy a week later at Southern Cross Hospital Christchurch. While I had two significant complications – ileus (where your bowel goes to sleep and doesn’t want to start functioning again) and atrial fibrillation (a common heart arrhythmia) – I was extremely lucky. My tumour was graded T3-N0-M0 and that was that. No other treatment required.
What followed was CEA blood tests every three months as well as colonoscopies and CT scans every year. Otherwise life went on as before.
I replaced my GP – although to be fair I never had any bowel-related symptoms.
When I passed the one year post-surgery mark I heard words of assurance – recurrence is apparently most likely in the first year after surgery. When I passed the five year mark I heard further words of assurance – five years is considered the time frame after which some people consider you cured of cancer. The CEA blood tests and CT scans eventually ended and the colonoscopies became fewer in frequency.
12 years flew by.
In the spring of 2023 I wasn’t feeling well. I was slowly alternating between mild constipation and mild diarrhoea. My GP prescribed loperamide.
Although I wasn’t due for my next colonoscopy until May 2024, I thought I should get things checked out so I went back to my surgeon. He scheduled a colonoscopy. That was smart on my part. What was incredibly foolish on my part was I had a scheduling conflict; I cancelled the colonoscopy and I failed to make a new appointment as my symptoms disappeared in the interim.
In October 2023 my atrial fibrillation acted up (first time in a long time) and I wound up in A&E. The emergency doctor sorted out my atrial fibrillation. But he also wagged his finger at me. “WHY ARE YOU ANAEMIC?” he asked rather strongly. “Your iron has been slowly declining over the past few years. I am going to give you an iron infusion before you leave but you need to find out the cause.”
ANAEMIA???? Off went the alarm bells.
So began Bowel Cancer Act II.
Finding out it was faster and cheaper than a conventional colonoscopy, I scheduled a CT colonography. This was completed within a couple of days of my A&E visit. The report was a shocker – the radiologist recommended an urgent referral for surgery as a tumour was located in my transverse colon.
I rang my surgeon’s rooms and told the nurse that I had just been diagnosed with bowel cancer – again. I was seen later that day by my surgeon and surgery was scheduled for the next week.
Same surgeon, same hospital, and same surgical procedure (more or less – this one was called an extended right hemicolectomy) made the situation feel quite surreal. One of the nurses at Southern Cross Hospital asked me if I found it comforting or terrifying that I knew pretty much what was about to happen to me. My answer then – as now – is a bit of both.
Just like in 2012 I had the same complications – several incidences of atrial fibrillation as well as ileus. I was transferred to Christchurch Public Hospital after nine days so I could be put on TPN while I waited for my ileus to resolve. Eventually it did resolve and I went home, about 15 kg lighter than when I entered hospital. My tumour this time was graded T2-N0-M0 so my incredible luck continued; despite my foolishness the tumour was removed in time and no further treatment is required.
The only difference in Act II is this time I was diagnosed with Lynch Syndrome. Lynch Syndrome is an inherited genetic disposition to various forms of cancer, most notably bowel cancer. Neatly explains why I’ve had bowel cancer twice. Might explain why I’ve had melanoma once. I’m adopted so there were no clues in my family that this was lurking in my chromosomes. My only child passed from complications from Prader-Willi Syndrome twenty years ago so no one is left for me to warn.
What does the future hold? Deja vu. Back to CEA blood tests every 90 days, colonoscopies and CT scans every year, and perhaps screens for other cancers associated with Lynch Syndrome (I’m unclear at this stage what those might be).
My reaction to all this? I’m bemused. At times I am a bit despondent wondering if I’m going to be playing “Whack-A-Mole” for the rest of my life, frantically screening for bowel and other cancers hoping to catch them early while they are still potentially curable. I’m amazed at how well my bowel function is with only ⅓ of my colon remaining and worry about what might happen if that last ⅓ of my colon winds up having to be removed in future.
Other times, I am stoic. I reflect on a comment a doctor friend of mine made. In reaction to my telling her about my diagnosis of Lynch Syndrome she said, “Well 1 out of every 6 people die from cancer. Lynch Syndrome or not, cancer and heart disease are the top two causes of death among older people” (which – being in my 6th decade of life – describes me). She’s not a counsellor (for good reason LOL) but her message made sense to me: Live life the best you can for as long as you can; worry changes nothing.
Bowel Cancer NZ very kindly referred me for counselling. This has been a tremendous help. While I’m still coming to grips with everything that has happened, I’m pretty much back to living my life as I was before. I am neither stoic nor am I crippled by worry (most days….). Usually I worry a bit, sigh, and reckon all I can do is follow my specialist’s advice and not be a fool again and delay any recommended screenings – bowel or otherwise.
I did switch GPs. Again. No particular reason this time; somehow it just felt like the thing to do given the incredible sense of deja vu Bowel Cancer Act II has carried with it.
Now if only the deja vu will continue and give me another 12 years before I’m in serious trouble again…”
Jodie’s Story

“Raising awareness is my mission now! It’s a scary thing to be told you have Cancer.
I was 44, owned a busy cafe, I was a Mum, and a Wife juggling the aftermath of the first COVID lockdown. I was once told life will only throw you as much as you can handle, well boy was this a lot to handle! My Uncle & My Dad both had bowelcancer, my uncle was only in his 30’s, my Dad was diagnosed in his 70’s with stage 4, 8 months later he passed. I procrastinated getting checked, partly because of dad’s horrendous ordeal, partly because I didn’t think my insurance would cover the colonoscopy and I didn’t qualify under the public health system. Instead of ringing my insurance I left it, thinking “I had no symptoms I’m fit and I eat well, it couldn’t possibly happen to me”.
About a year later I started feeling tired, I was working 60 hours a week of course I was tired, we
went into covid lockdown and my thoughts went to keeping my business going. When lockdown
restrictions were lifted and business started to pickup I ran into a friend. His wife, pregnant with
their second child had just been diagnosed stage 4 bowel cancer and instantly I thought “she’s
too young!” then timed with the bowel cancer advertising I decided I needed to get checked. By
this stage I had started to have some irregular bowel habits which i put down to maybe
haemorrhoids, not enough water, not eating enough fibre etc… my symptoms were minor, minor
enough for some to ignore, but I had a nagging feeling something wasn’t right.
I went to my GP or promptly made a referral for a colonoscopy, I was fortunate that he acted and that I had private health insurance. Two weeks later I had the colonoscopy and a 10cm tumour removed, I will never forget my specialist calling me, he said “do you want to come in or would you like me to tell you over the phone”. I’m not a patient person and the anxiety of not knowing would have been unbearable, so I said “I would like to know now” he said “I’m really sorry Jodie but it’s Cancer”.
Me being me straight away my thoughts when to “what do I need to do to fix this?” I had an
appointment that afternoon with him and we discussed my options. Surgery was my best option
so within 10 days I found myself on a hospital bed awaiting bowel surgery to remove 1/4 of my
bowel. Once removed it when for testing, It was a long anxious wait for the results, although only
2 weeks it felt like months. I got the news that it was Stage 3B, Cancer had spread to lymph
nodes and chemo was now a reality.
I knew very little about chemo treatments, I thought my hair would be gone! I was terrified. Up until now I hadn’t told many people, losing my hair wasn’t a vanity thing, it would mean having to tell people and I didn’t want to have people feeling sorry for me or sharing their stories of their aunties cousins cousin… If I’m honest denial was a factor, to talk about it over and over would mean it was real! I thought I could handle this on my own, with very few people knowing …. So I went to my first oncologist appointment and my options were given, I opted for 4 cycles infusion & tablets and with a few tweaks along the way I was able to continue working and my ordeal went mostly unnoticed.
Don’t get me wrong it was far from easy,
there were days I just wanted the earth to swallow me. Once chemo was over, there was never a
celebration, there was no sense of closure. I tried to get back to “normal” but I always felt like I
was never going to be “normal again. Mentally, emotionally and physically drained, all the bottled
up stuff was beginning to bubble out the top and I often felt like I wasn’t in control anymore. I’ve
never been one to dwell so I knew had two choices, sink or swim. I chose to swim, I focused on
my business, and managed to get that thriving again.
Although I continued with routine blood tests, I still couldn’t get the constant fear of whether it
was gone or if it would come back. I asked my Specialist if I could have my yearly CT scan early, I
felt fine, no symptoms but I just had that niggly feeling! I got my Scan early, there is no words to
describe the anxiety you feel leading up to a scan! On the outside I’m outgoing Jodie but on the
inside I’m a scrambled mess of emotion. I had my scan and usually I would get results within 2
days, but I heard nothing, so I chased up the surgeon and his receptionist said he was really busy
and would ring! 6:30pm on a Friday night he rung, there was a suspicious nodule on my right
lung, my heart sank, he was as surprised as I was so to be sure he sent me off for a PET scan.
That too noted it was suspicious, so I had a meeting with the thoracic surgeon and decided that
surgery would be the best option. So once again I was faced with major juggling with staff and
cafe commitments. On the 9th September I underwent a lobectomy to remove the middle portion
of my lung. 2 Days after surgery we went into lockdown for the 2nd time! In a way this was good
as I didn’t have to stress about the cafe while I was recovering, I just kept thinking wow if I hadn’t
asked for my scan early how much would the delay have impacted the outcome.
My Results came back clear so no need for more chemo! It was a relief. I count every day as a blessing and everyday feels more and more real! I am truely privileged to be here to share my story, It has taken a while but I now feel comfortable talking about cancer and I decided it was important for me to speak out, to raise awareness.
Nearly 2 years one another cancer was discovered in my lung, thankfully it was just a wedge resection and no lymph nodes were affected.
I now speak up in the hope that my story will change someone’s else’s story. As part of a wider research committee I joined the Australasian Gastrointestinal Cancer Trial Group (AGITG) as a Community Advisory Panel member, to give patients a voice in clinical trials.
Nobody likes to talk about their bums, but talking about it could save yours or someone else’s.”
Victoria‘s Story

Victoria Thompson
Victoria Thompson is Bowel Cancer NZ’s Nurse Support Coordinator. An experienced Registered Nurse, Victoria sees her role as an amazing opportunity to help patients and whānau through nursing support, education and advice, and to help increase awareness of bowel cancer.
Her role mainly includes supporting those who have been diagnosed with bowel cancer or their close family members through our confidential nurse support service. Victoria also administrates the Bowel Cancer NZ’s patient support group, a closed Facebook group for those who have been diagnosed with bowel cancer and their whānau.
“Through my previous work in palliative care, I had noticed Bowel Cancer NZ’s outreach within the community, through education and awareness. People are talking more about bowel cancer now – thanks to the screening programme and awareness of the support available. The work Bowel Cancer NZ is doing is already making a difference and that’s only going to grow.”
Victoria believes the screening programme has really helped raise awareness of bowel cancer and helped people overcome the stigma if they do get it. “Having it highlighted regularly in the media has helped – it’s been good for New Zealanders and led to an even greater need for our services at Bowel Cancer NZ.”
“I’m meeting younger and younger people being diagnosed with bowel cancer all the time – those in their 20s or 30s. It’s really tragic. Part of our remit is to help GPs become more aware that young people can get bowel cancer too – it’s not just an older adults disease.”
“My advice is that if you’re worried about your symptoms, even if they only seem minor, go and see your GP,” she says. “Some people may find it embarrassing to talk about their bowel issues, but it’s your health on the line – and your sanity. Your GP can run some very basic tests and follow these up as and where needed.”
Victoria is a ‘people person’ who loves helping others. Warm, approachable and easy to talk to, she says she’s only ever had ‘the best’ patients and families. “If you’ve been diagnosed with bowel cancer, or someone you love has, don’t be afraid to reach out for support,” she says. “I can point you in the right direction, help you figure out all that confusing bowel cancer terminology and the effects of different treatments – and even help you work out what to say to your family. Just email me: I’m here to help.”
Victoria is available to talk to on our 0800 BCNZ NURSE (226 968) number as well as via the live Chatbot on our website.
Dr Mathieson’s Story

Anne Mathieson
Dr Anne Mathieson is a 36-year old GP, and mum to two young children – and has been a bowel cancer patient. This means she can offer a unique perspective as a medical advisor.
Anne was diagnosed at just 34 years old and says it came as a real shock. She had symptoms of bleeding for a few days once or twice a year, for about six years. She was told she likely had haemorrhoids, which seemed like the obvious answer due to her age and no other apparent red flags.
Around a year after the birth of her second child, her symptoms became more persistent, so she requested a referral to a specialist, but had to wait a couple of months for her appointment. Following the examination, Anne says the specialist “became very serious” and she was sent for an urgent colonoscopy. Several polyps were found and removed, with the largest one having cancer. Due to the margins on the cancerous polyp being too small and the number of other polyps in the remainder of the bowel, her whole bowel was removed shortly afterwards. Following surgery, the histology demonstrated that there was microscopic disease in two of the removed lymph nodes meaning her cancer was upstaged to early Stage 3 and she proceeded to have three months of chemotherapy.
Anne had a ‘gut feeling’ that something wasn’t right, so she asked her husband to come to the specialist appointment. Being a GP made her more aware of her symptoms, and she says she became very impatient about waiting two months to see a specialist, but at that time, everything else seemed normal.
Physically, Anne is now feeling very well, but emotionally, she says it has been a very tough year. She now has regular tests and CT scans, as well as three-monthly blood tests, plus she’s taking part in a ground-breaking University of Otago study, in which they have sequenced the tumour DNA to then look for circulating tumour DNA in the blood. The goal of the study is to better personalise disease monitoring to detect any recurrence earlier in order to improve the prognosis if there is a recurrence.
Anne was inspired to become a medical advisor to Bowel Cancer NZ, not only because of her personal journey but to add another dimension to her work as a GP. She is part of a worldwide network of doctors who have had cancer, and she was offered some career counselling through them. “I realised I wanted to do something significant that makes a difference – and I feel I can offer a unique perspective, being both a medical practitioner and a patient,” she explains.
“The roll-out of New Zealand’s national screening programme is really promising, but it’s not enough,” says Anne, “There is a lack of funding around bowel cancer for doctors to access investigations when patients don’t fit the boxes required to be seen,” – something she’s hoping to address. “I know when I look at my symptoms, there were no red flags and I was only seen when I was due to my resources and knowledge,” she says.
“Diagnostic services need to be more accessible, particularly for younger people. A diagnosis of bowel cancer always comes as a shock, because our mindset is that it’s not meant to happen to young people – but the reality is, it’s getting more common.”
Anne believes that the support of complementary care during treatment and the emotional recovery after cancer is not well addressed in New Zealand. “More doctors need educating about providing holistic care during treatment, helping their patients recover emotionally and she feels Doctors need to push the importance of exercise, which has the most evidence for reducing the rate of recurrence following treatment.”
She also points out that the symptoms of IBS (Irritable Bowel Syndrome) and bowel cancer can be remarkably similar. “Many patients have IBS and self-diagnose or learn to manage it through diet and lifestyle. But if you have any symptoms which aren’t settling, just go and get checked, even if you think it’s ‘nothing’. Trust your instincts if you have a gut feeling: push back and ask for more tests. And if someone else tells you to get something checked, listen to them.”
Dr Crengle’s Story

Sue Crengle
Dr Sue Crengle is an Invercargill GP and a Professor (Hauora Māori) at Otago Medical School’s Department of Preventive and Social Medicine.
She specialises in general practice and public health medicine and has been working as a researcher for over 25 years. Much of her work involves identifying where and how inequities in our health occur and in testing ways to eliminate these inequities.
Dr Crengle strongly feels that bowel cancer is one of these inequities. “Bowel cancer is increasingly becoming an important issue for everyone in New Zealand. In the past, it’s been less of an issue for Māori, but now that’s changing.”
Sue points out that approximately 22% of Māori are diagnosed with bowel cancer before the age of 60 (compared with around 11% of non-Maori), yet the national screening programme doesn’t begin until 60 years (up until 74 years). “If we were to screen and diagnose Maori from 50 years of age, it would certainly make a difference. I’m really keen to see the screening programme provided more fairly – currently, there isn’t an equitable delivery of the programme.”
Dr Crengle says that since she moved to Southland over five years ago, she sees patients who are diagnosed with bowel cancer. “Southland has one of the highest rates of bowel cancer in the country, and it’s not yet understood why this is. I’ve had a number of patients diagnosed with bowel cancer, and sadly, a couple of them have passed away. Others have had it treated and are living healthy, happy lives.”
By serving as an advisor to Bowel Cancer NZ, Sue hopes to contribute a GP’s point of view and expertise. “My goal is to see equitable opportunities for everyone to benefit from the screening programme. I aim to provide more of a voice for Maori in particular, as well as about bowel cancer in general and how our health system is responding.”
Sue believes the national screening programme needs to continue rolling out across New Zealand and fast. “Screening is one of the best ways to reduce bowel cancer in our community: firstly, to have polyps removed before they can become bowel cancer, and secondly, to have any cancer identified early. But, like other cancer services, screening stopped during lockdown. Catching up with testing is really important – there’s a huge backlog, not only of people who haven’t received tests but also those who tested positive and need further investigation.”
When asked what advice she has for patients, she says, “If you’re sent a screening test, do it. And if you notice any changes in how your bowels work, any bleeding, stomach pains or other symptoms, then get them investigated early. Often it’s not bowel cancer, which is good to know, but if it is, then the sooner we can find that out, the better the outcome.
“Most of all, if you’re concerned about your doctor’s diagnosis, keep going back or get a second opinion until you get an answer.”
Kat’s Story

Katherine
Katherine (Kat) was one of the many Kiwis considered ‘too young’ to have bowel cancer – she was diagnosed at age 34. “My only initial symptom was fatigue. I had two kids at the time, so I saw my GP, who said my iron levels were really low and prescribed iron tablets.”
Over a year later, after Kat had her third child, she began to get constant pain in her abdomen. She went to three different GPs, who diagnosed indigestion and other ailments. By February 2015, she was in Auckland on holiday, when she had severe abdominal pain and could feel a ‘mass’ in her abdomen. She went to A&E and got sent straight through for a CT scan.
Kat had an operation the next day in Auckland to remove a large tumour in her bowel. Two weeks later, she flew back to Dunedin, where her oncologist told her she had incurable cancer. I thought ‘I’ve got 3 kids, I can’t have bowel cancer’. “It was Stage 4 cancer, she says. “I asked if I was terminal and he said, ‘no, you’re not in the process of dying – you’re in the process of living’.
She started on a combination of chemotherapy drugs, including an unfunded drug that cost $25K for 12 rounds. “After the first 12 rounds, it’s free, so I took it for four years,” she says. “I lost track of how many treatments, but they worked and my tumours kept shrinking.” In fact, Kat’s been in remission for almost a year. “It’s my five-year ‘cancer-versary’ on 15th February – for someone who’s had Stage 4 cancer, that’s amazing.”
“I’ve had a lot of support along the way, particularly from Bowel Cancer NZ, she says. “Mary (at Bowel Cancer NZ) provided me with one-to-one support and explained all that they do to help people get through this horrible diagnosis. It’s quite hard at first, people didn’t want to talk about, but I did want to talk about it.”
Mary recommended Kat join Bowel Cancer NZ’s support group for patients and their families through Facebook. “It really helped me to get feedback, support and advice from others who’d been there and done that. Mary also referred me to a counselling service through their Service Directory for my eldest son, who has anxiety and doesn’t like to be away from me.
“Most of all, you learn you’re not the only one going through this,” she says. “At times, you can feel very alone and very isolated, but Bowel Cancer NZ really reaches out to help you.”
Brad’s Story

Brad
My journey started when I came down with a bit of headache and felt lethargic which was out of the ordinary for me. I was 28 and had never had a sick day in my life but felt so bad that I ended up in bed for 3 days. Each day was getting worse, I had no energy at all and was starting to turn yellow. By this stage my wife booked me into the doctors so after some blood tests I was rushed to hospital and ended up spending two weeks in isolation there while they tried to figure out what was wrong with me. I lost 12kg in my first three days in hospital and literally didn’t have enough energy to speak or open my eyes. It was probably the scariest time of my whole journey as no-one could find why I was so sick. Fortunately for me I was placed under the care of the amazing Frank Frizelle during this time.
After my eventual discharge I slowly started to feel better in myself but also started to show some classic symptoms of bowel cancer. I couldn’t put any weight back on, I had blood in my stools, and I had the most intense stomach pains I had ever known. Repeated trips to my local doctors followed but everyone brushed it off as side effects of the still undiagnosed illness and treatment that I had recently had, as well as the myth of not being able to have bowel cancer as you’re too young. Finally I had a follow up appointment with Mr Frizelle where we discussed the symptoms I was experiencing and he organised an urgent colonscopy for me.
Waking up from the colonoscopy I was told that they had discovered a tumour in my colon. From here things started moving pretty fast, I was booked in for surgery in 2 weeks time, had numerous scans, more blood tests, colostomy bag training – it felt like I was a the hospital for something every day. As funny as it sounds it actually was a relief to know what was wrong with me and to have a plan in place to get better. I had spent plenty of nights awake worrying that I had bowel cancer, now that I knew I did it was easier to get on with treatment. This diagnosis also provided answers to why I had been so sick, a simple virus had entered my bloodstream because of the tumour and amplified the effects. At this stage everyone was under the impression that it had been detected early and would probably only need surgery so I was in a pretty good headspace at this time.
However, 3 days after surgery I was diagnosed as Stage 4 as the tumour had penetrated the wall of my bowel and had spread to my lymph nodes so some pretty aggressive treatment was planned. My first meeting with my oncologist was without doubt the most confronting thing I have ever been through. He deliberately didn’t talk numbers with me but also left us in no doubt about how serious the situation was. I started my chemo one week after that meeting and had 8 rounds of a 3-week cycle. The chemo really knocked me around but I found setting little goals for the end of each cycle really helped. Sometimes it was as simple as taking the kids out for dinner or going away for a night as a family.
Following the end of my chemo I was on regular checkups and scans. I found the scans and waiting for results really hard. During this time was when I’d start to think the worst and I would be really dreading the results. I downplayed my two-year scan as I felt as though I was tempting fate, however after I had my 5 year scans it felt like somewhat of a weight had been lifted. I’ve now just ticked over 9 years and am incredibly appreciative of my situation and realise how fortunate I am. I personally think the biggest challenge in cancer is the mental battle, not the physical one, and would recommend to everyone to open up and talk to someone about how you feel rather than try to shoulder the burden yourself. Everyone close to you is suffering as well but most of us have a tendency to bottle things up.
Prof Frizelle’s Story

Frank Frizelle
Professor Frank Frizelle is a bowel cancer specialist, Professor of Surgery, the Editor in Chief of the New Zealand Medical Journal and he is also one of Bowel Cancer New Zealand’s medical advisors.
Frank treats people with bowel cancer almost every day and spends a lot of time researching causes, treatment and outcomes. “Most bowel cancer is sporadic, not inherited,” he says. “And in fact, less than 10% of bowel cancer is likely associated with a inherited genetic predisposition , so the way you live does have an impact. Exercise is good for you for many reasons, including weight control. Healthy living definitely makes a difference, but then young, fit people can also get bowel cancer.
That’s why if you have any symptoms, it’s vital get them investigated, no matter what your age,” he says. “And keep getting checked if you’re not happy with the diagnosis. Many bowel cancer symptoms fluctuate – they can come and go – so it always pays to get checked if anything is bothering you.”
Frank has been advising Bowel Cancer New Zealand for a few years and is very proud of the work they do in advocacy, research, education and patient support. “Bowel cancer is New Zealand’s second highest cancer killer. So our advocacy work in getting home screening kits off the ground is already helping to save lives. But there’s still so much more work to do.”
Frank believes education is key, particularly for men, older people and those who live in rural areas. “It’s fantastic that New Zealand is now rolling out home screening kits, but so far it’s only reached about half the population – it’s not happening fast enough. The people we’re failing are those who are in rural locations or not well off – they just aren’t aware of the symptoms of bowel cancer. So it’s about spreading the word in those areas. And many older people aren’t Internet savvy, so it’s important to get the message out there too.”
Recently, Frank led a research team that discovered links to bowel cancer from a toxin producing carried in the gut. This discovery means that people can be screened for the bug and a lifesaving treatment can be developed – a world first. In 2018, Frank received the NZMA’s highest accolade, the Chair’s award, for his outstanding contribution to health in New Zealand.
Karen’s Story

Karen
My Journey
In February 2015 I was at the doctors with my daughter, on the way out, literally half way out the door, I mentioned that I had been suffering from quite (no in reality very severe – think take your breath away) lower abdominal cramps. I had assumed that they were all part of the wonderful menopause process. Not so said my doctor and thankfully requested that I have a scan as soon as possible as they could have been the result of an Ovarian Cyst.
On the 9th of February I had this scan and wondered why the technician was looking very worried and not speaking that much. Following this, I had a call from my doctor’s office asking me to come in that afternoon (this – as you can image seemed very abnormal and quite distressing). On arrival, he asked my three children to remain in the waiting room (also raising alarm bells), and then told me the devastating news that I had bowel and liver Cancer.
By 9.00a.m. Thursday of that same week, my wonderful doctor had organised and streamlined for me to have numerous blood tests including a colonoscopy, MRI and an appointment with an amazing oncologist. (this may not seem a lot to the uninitiated however to get bookings for these types of tests and specialists can take weeks if not months – wake up call to me – this is serious).
My oncologist, with all family present, then told me I had stage 4 bowel cancer that had metastasised to my liver and lung. I was told that my survival rate was 40% and I would need chemotherapy and three major operations. They estimated that my cancer had been present for 7 years, given how large the tumour in my bowel was and the five tumours in my liver. To give you an idea of how obtrusive this is, a paediatric colonoscope had to be used in lieu of an adult one.
Here I digress slightly. Yes, I had signs to warn me of what was happening, however I am one of those people that don’t like going to the doctor unless it is for my children and definitely don’t enjoy the thought of taking a ‘poo’ sample or having a camera put somewhere that it definitely should not normally go. Both fears are ridiculous, our wonderful health care professionals are used to ‘these’ samples and a colonoscopy is absolutely nothing to fear or be concerned about. NZ’s rate of bowel cancer is higher than that of prostate or breast cancer and therefore ensuring you have a colonoscopy once every three years can detect and prevent this insidious disease doing what it did to me – spreading to my liver and lung and hopefully nowhere else, but we don’t know that yet. SO PLEASE, if you have the slightest symptom – get it checked, it is not embarrassing, it does not hurt and it may keep you alive to watch your children grow up.
A second part of my digression is my wonderful surgeons and oncology treatment – it is expensive – please get health insurance as this made my horrible journey a little bit more comforting – these people are with you 24/7, they were my saviours and all three of them saved my life, more than once – so many stories, not enough time – but heroic stuff.
Treatment started:
Schedule was – three months chemo, bowel operation, liver operation, 3 months chemo.
Unfortunately, I ended up having to have 6-months of sessions of chemo – HELL (will explain later) followed by two very major operations.
When I began this journey my CEA (cancer levels) were 148, they are now 1.9, which is normal, we all have between 1-4 CEA levels in us.
So, the reasons for the above, my oncologist recommended in my chemo treatment a new drug called Avastan – it was super powerful and its only downside was that it could cause blood clots and that it was not yet funded so was expensive, however my family who are my lifeline were right behind me in helping me to get this treatment. After my fourth chemo treatment I became very short of breath and my normal physical activity was simply out of the question. Fitness was my reason for living and the reason I lived. I could not even walk up a flight of stairs or up the sand dunes from my beloved beach. One afternoon, after a weekend of feeling very very unwell, I had to get out of the house and so went to the movies with my daughters and went to lunch prior to the movies, unfortunately we never made it to the movies, half way through lunch my daughters voices faded and my life blurred into a black nothing. I came back from this (although apparently I should not have), the two massive blood clots on my lung and right by my heart should have, nearly did, kill me. The reason according to my doctors that I survived was my fitness levels – PLEASE ALWAYS STAY FIT, no matter how hard, when you are going through chemo, even if it is a ten minute walk with frequent stops which I did often, it is the best thing as opposed to lying in bed.
I then went to another wonderful specialist, a haematologist, who prevented this from happening ever again. Because of these blood clots, I had to continue with the chemo rather than have the surgeries as planned, hence the 6 months of chemo. All of the people at my oncology department at 161 in Epsom could not believe that I could continue 6 months every fortnight without a break – I worked through this entire time and kept trying to exercise – which was probably the only reason I got through. I was stubborn and with the love and support from my family, I got through the 6 months.
So now the surgeries, bowel first.
The tumour in my bowel was so large that the colonoscopy camera could not get past it, nor could the child’s camera ugh!!! I had 20cm of my bowel and a lymph node removed, my surgeon was nothing short of a SAINT! Following the surgery, I thought I was all good to go after 3 days, not so, fourth day I got sicker and sicker – it was very very bad – my surgeon (who was sick himself) came in at 3.00 a.m. to put a nasal gastric tube in as none of the nurses could get it in due to a failed nasal operation in my youth, he got a scan on my surgical wound and they said it was fine. He questioned this result as I was so ill, if he had not I would have died as it was slowly leaking and would have caused peritonitis. Back into surgery. re-opened, restitched and given a colostomy bag – MY WORST NIGHTMARE – to let the bowel heal. This was only temporary. Intensive Care for 2 days and again saved by my fitness levels.
Liver surgery – another amazing world leading surgeon – so lucky. He had done a portal vein embolisation early on in my chemo (April) which basically shut down the blood supply to the larger part of my liver (we have a large blood vessel running through our liver and fortunately for me my tumours were all on one side of this vessel) so it basically died, leaving the smaller 30% part to think whoa, need to grow right now so by the time I had my surgery in November my 30% had grown enough to allow my surgeon to remove 70% of my original and diseased liver. Sounds simple right? It hurt like hell, as they literally have to angle out your rib cage to get to your liver and that recovery hurts argh!
But your liver is amazing – it completely regenerates – it is truly amazing. Mine is all brand new, pink and pretty (silver linings right?).
Oh, and at the same time as executing the liver surgery they removed the ‘HORRIBLE’ bag.
Well, that was it I thought, I had ongoing scans, blood test and colonoscopies and all was fine until Feb 2017 (two years later) and my CEA levels went up and everybody went into panic mode, including me. It was back – in my lungs.
By this time my wonderful oncologist had retired and the results I received from my new oncologist did not please me – stubborn – I rang my old oncologist and he explained, thankfully, that the tumours in my lung were there all along. Despite their presence, they were small and passive-growth tumours. Accordingly, they decided to treat the two major areas of concern – my bowel and liver – and treat the lung tumours at a later stage.
So, another operation – BUT NO CHEMO – and half a lung removed. By half I mean one lobe – your left lung comprises two lobes, your right has 3, and I had my top right lobe removed.
The ongoing treatment is that you have 3 monthly blood tests, 6 monthly scans and 2 yearly colonoscopies. At my last colonoscopy, which I have to stop my eternal Pradaxa (to stop blood clots) for, I was perhaps told to resume my Pradaxa a little early – my warning is – don’t! A week after my colonoscopy (at which had had a slight bit of bleeding but nothing serious so thought nothing of it) I went to work, had a meal with a glass of wine and then started to feel a little tired – I ended up passing out on the floor and haemorrhaging nearly 4 litres of blood and being rushed to hospital (thanks to my daughter hearing my cries for help) with sirens blaring and a Code 1 blasting over the mobile to the hospital.
I tried to remain positive throughout my journey and tried to stay as fit as possible, even though I was constantly reminded that I only had 40% chance of surviving, I thought those were pretty good odds.
Sometimes you just stop, sit and think … F..k I have been through a lot of shit but I am alive and hope to stay that way. For anybody out there, recently diagnosed or going through treatment – Kia Kaha – stay fit, stay positive and if you need to talk to anybody I am happy to talk to you so please do not hesitate to reach out.
I just want to make sure that anybody that has the symptoms – please get them checked, I didn’t, don’t make my mistake.
KAREN HART